As the largest legacy hospital in Singapore with numerous
global awards under its belt,
Singapore General Hospital's journey is one of medical excellence. Currently,
liver transplant is one of SGH's key services, where SGH's Transplant programmes perform the highest number of transplants in the country.
Established in 2005, the Liver Transplant programme brings together various specialists from the cluster including
hepato-pancreato-biliary/transplant surgeons, hepatologists, infectious diseases specialists, and allied health specialists into a multi-disciplinary centre to provide holistic care for patients with liver disease and require liver transplant.
Care is organised around the patients and their needs, where patients have the convenience of seeing their doctors in the same place.
Services Provided
We offer a full range of comprehensive services related to liver transplantation including:
- Adult living liver donor liver transplant
- Blood group compatible and incompatible
- Small for size graft
- Pure laparoscopic donor hepatectomy
- Combined solid organ transplant
- Pre transplant recipient assessment
- Liver donor assessment Pre and peri liver transplant management
- Lifetime post transplant follow up care
- Post living liver donation care
On top of that, patients will receive full access to supportive care from multi-disciplinary team.
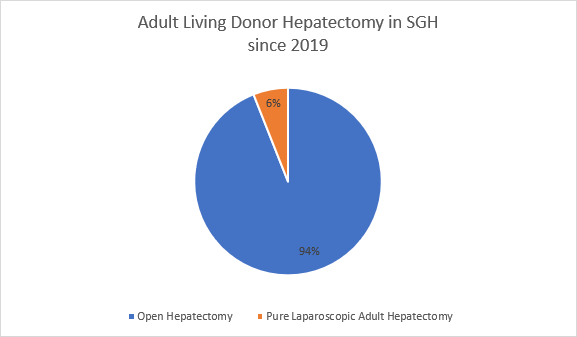
Pure Laparoscopic Adult Donor Hepatectomy
One of the major milestones was the introduction of pure laparoscopic adult living donor hepatectomy in 2019.
At the moment, SGH is one of the leading centres in the region for pure laparoscopic adult living donor hepatectomy where 94% of our living donors underwent laparoscopic hepatectomy since implementation.
Several advantages of laparoscopic living donor hepatectomy are:
- Faster recovery
- Improved cosmetics
- Lower postoperative pain
- Lower rate of hernia incidence
- Less adhesions
- Reduce length of stay
SGH deploys its highly experienced surgeons to master the challenges and tackle the complex techniques of laparoscopic liver surgery. SGH HPB surgeons have vast experience with over 1,200 laparoscopic liver resections and annual volume of 140 -150 laparoscopic liver resections per annum.
Since inception, zero living donor mortality has been reported at SGH and our surgeons are committed to hone their surgical skills in the hopes of improving patient outcomes and experience.
Laparoscopic paper: A systematic review and network meta-analysis of outcomes after open, mini-laparotomy, hybrid, totally laparoscopic, and robotic living donor right hepatectomy.
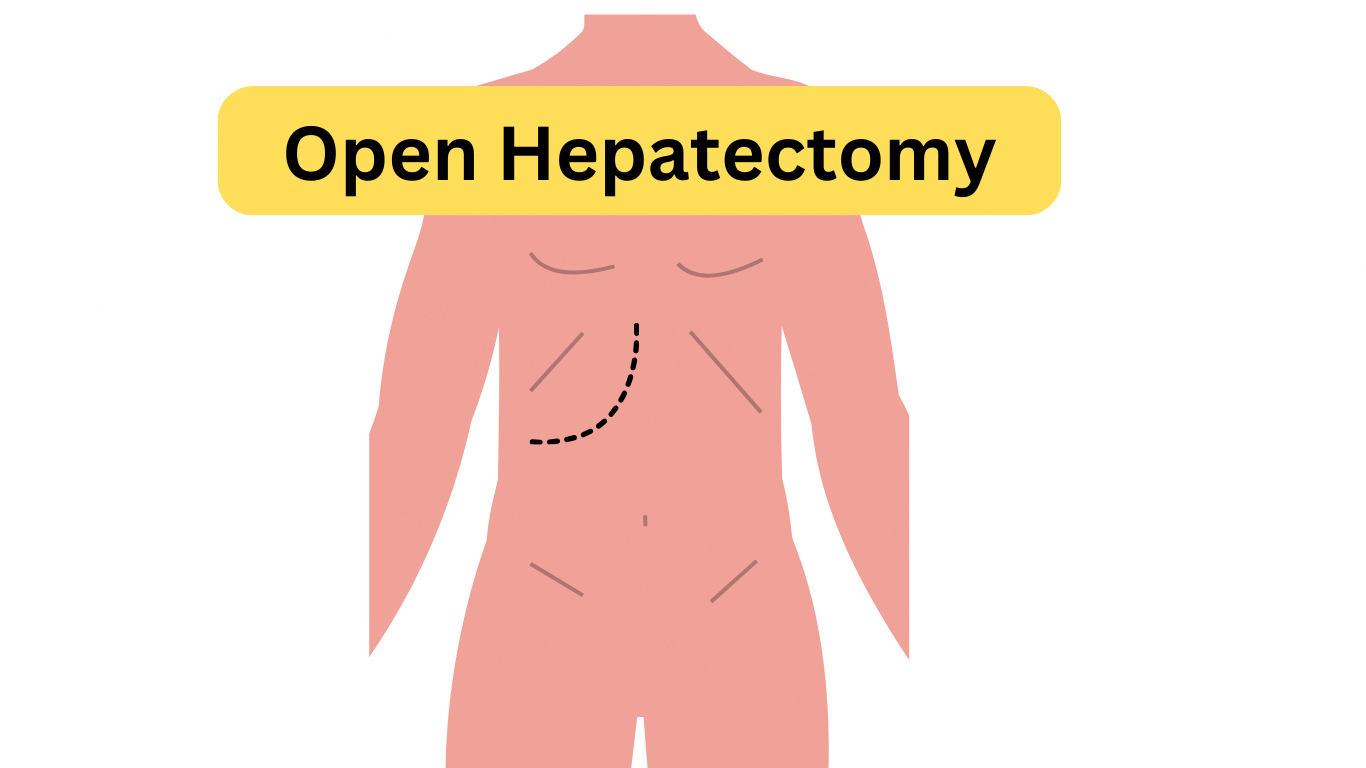
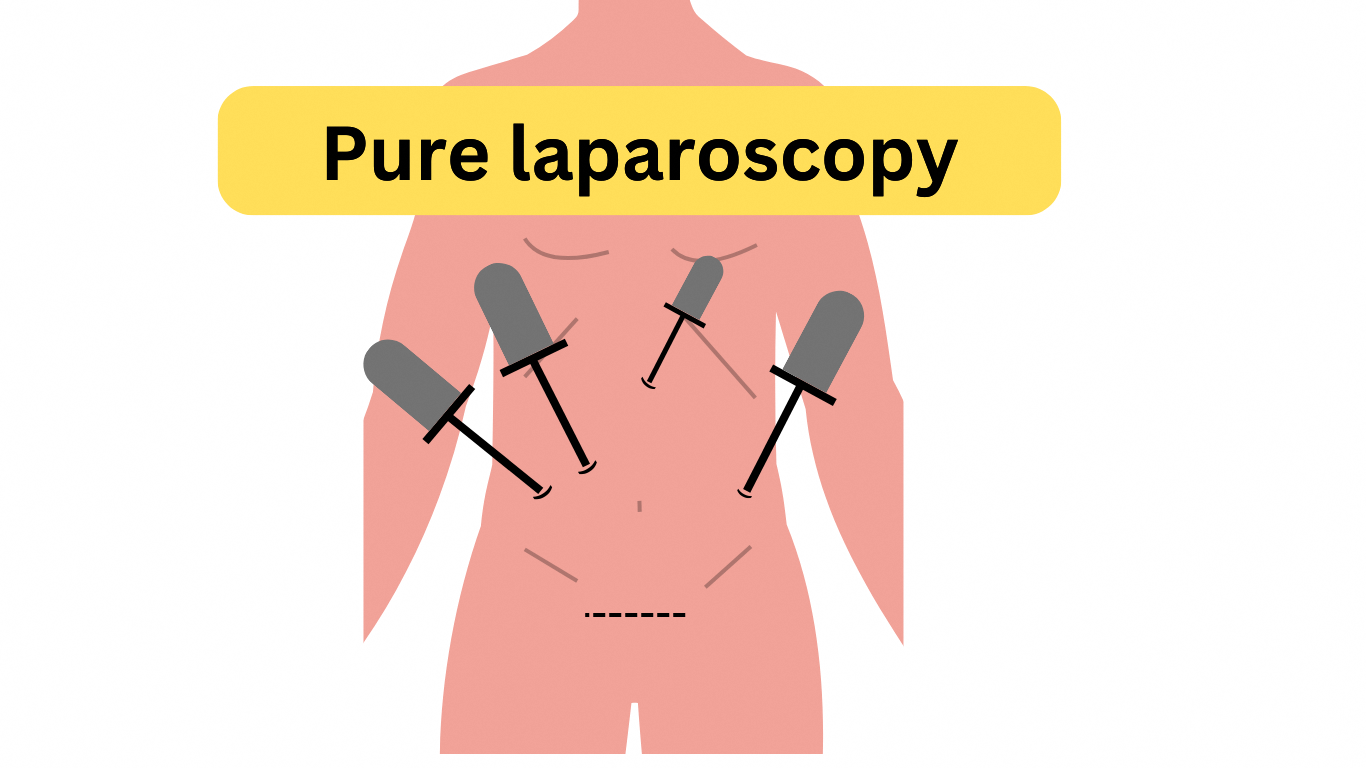
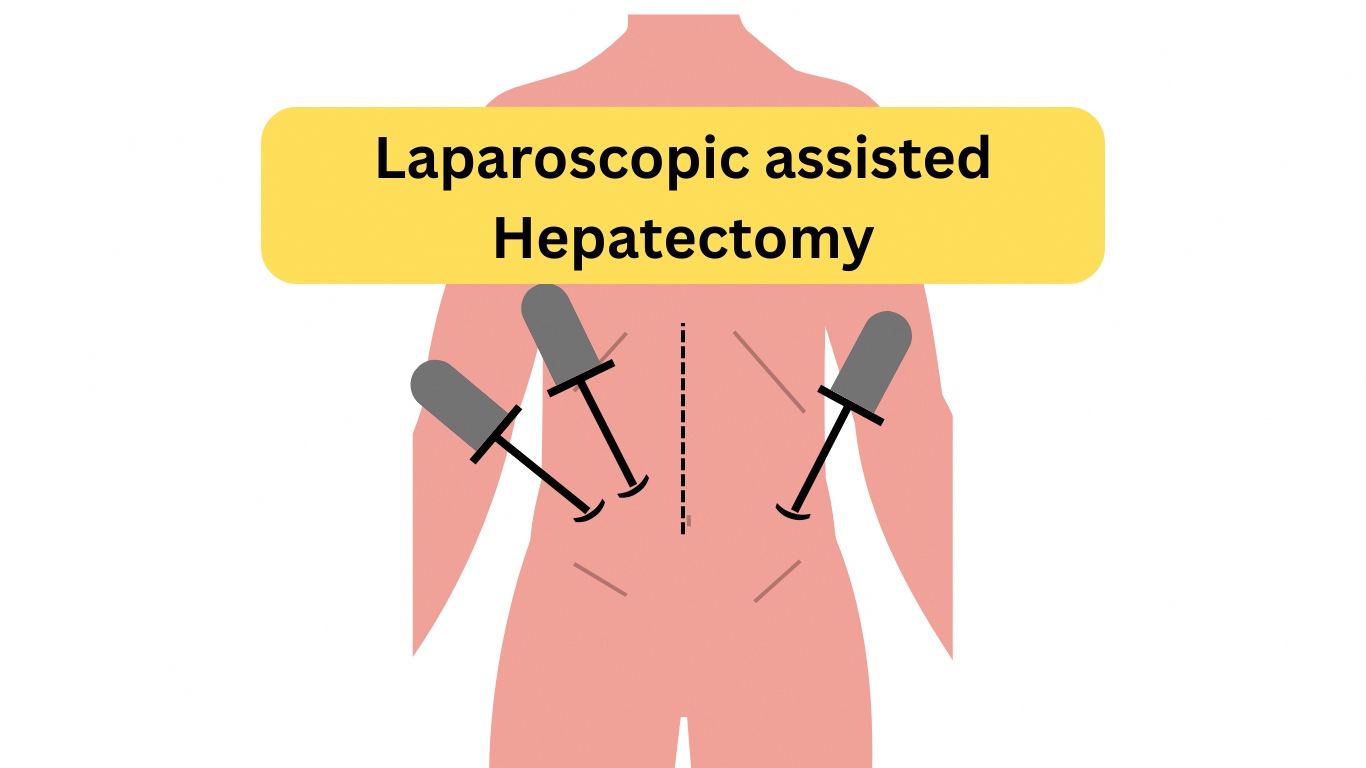
Living Donor Hepatectomy in Pictures
SGH Liver Transplant Programme Milestones
- 26 Mar 2022 – 1st Living Donor Intestinal Transplant in Singapore
- 19 Mar 2019 – 1st Laparoscopic Living Liver Donor hepatectomy in SGH
- 18 Jul 2017 – 1st ABO-incompatible transplant in South-East Asia
- 8 Apr 2009 – 1st combined heart and liver transplant in the region
- 15 Feb 2006 – 1st Deceased Donor Liver Transplant
- 22 May 2006 – 1st Living Donor Liver Transplant
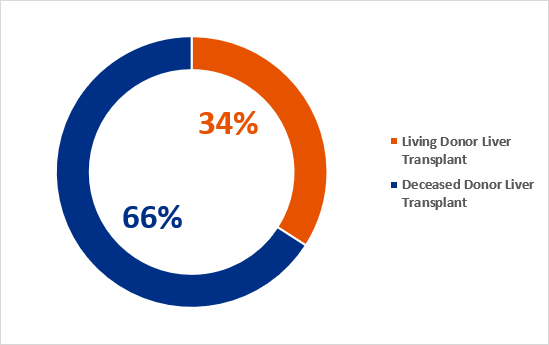
Current Stats
- In 2023, 100% 1-year recipient survival
Our multi-disciplinary team (Surgeons, Hepatologists, Infectious Disease Physician, Endocrinologist and Allied Health Professional etc) is devoted to improving patient care and transplant outcomes.
Transplant Outcomes
The following data presents SGH's liver transplant outcomes compared to international benchmarks, focusing on patient and graft survival rates for both deceased and living donor transplants. The analysis includes 1-year survival for benchmarked cases and 5-year survival for all cases.

| 1-year survival for benchmarked cases* | 5-year for all cases# |
|---|
| Deceased Donor | Living Donor | Deceased Donor | Living Donor |
|---|
SGH Patient Survival, 2015 - 2023 | 96.8% | 100.0% | 86.1% | 71.9% |
International Benchmarks | 91.6%3
| 90.9%4 | 81.4%1 | 70.0%2 |
SGH Graft Survival, 2015 - 2023 | 96.8% | 100.0% | 86.1% | 72.0% |
International Benchmarks
| 89.0%3
| 92.3%4 | 79.3%1 | 62.0%2 |
#Analysis for five year includes all cases.
*Analysis for one year only includes SGH benchmarked cases.
For DDLT: benchmarked cases 56.1%
For LDLT: benchmarked cases 40.0%
DDLT inclusion criteria for benchmarked cases
(include patients transplanted between 2015-2023 who fulfil this criteria)
| LDLT inclusion criteria for benchmarked cases
(include patients transplanted between 2015-2023 who fulfil this criteria) |
|---|
- MELD < 30
- BAR ≤ 9
- No previous biliary / liver surgery
- No portal vein thrombus
- Not in acute liver failure/require ventilation
| - MELD <20
- No portal vein thrombosis
- No previous major abdominal surgery
- Not in acute liver failure,
- Not admitted to the ICU or needing renal replacement therapy / dialysis or ventilation at time of transplant
- No inflow modulation/ small for size graft
|
LDLT exclusion criteria
(exclude patients transplanted between 2015-2023 who have this) |
|---|
- Cases with biliary atresia, previous major surgery (ie colon, stomach, biliary surgery, liver /wedge resection)
- Graft weight ratio <0.8
|
Legend
DDLT: Deceased Donor Liver Transplant
LDLT: Living Donor Liver Transplant
1 Organ Procurement and Transplantation Network (OPTN)/Scientific Registry of Transplant Recipients (SRTR) 2021 Annual Data Report: Liver, American Journal of Transplantation: Official Journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2023; 23(2S1): pp. S178–S263
2 Living donor liver transplantation in Europe HepatoBiliary, Surg Nutr 2016; 5(2): pp. 159-175
3 Defining Benchmarks in Liver Transplantation A Multicenter Outcome Analysis Determining Best Achievable Results, Annals of Surgery 2018; 267(3): pp. 419-425
4 Novel Benchmark for Adult-to-Adult Living-donor Liver Transplantation Integrating Eastern and Western Experiences, Annals of Surgery 2023; 278(5): pp. 798-806
SGH Liver Transplant Team
The SGH Liver Transplant Programme is led by a multidisciplinary team of specialists, including transplant surgeons, hepatologists, infectious disease physicians, and allied health professionals. Key leadership roles include the Transplant Program Director, Deputy Directors for Medical and Surgical aspects, and the Liver Transplant EXCO.
Media Engagement
The Liver Transplant Centre actively engages with various media platforms to educate the public about liver health, transplantation procedures, and organ donation, aiming to raise awareness and promote understanding of this critical medical field:
Watch this space for more updates.
Liver Transplant Resources for Patients
Our webpage serves as a vital knowledge hub for those navigating the complexities of liver transplantation. This extensive collection of materials offers insights into every aspect of the transplant process, from initial evaluation to long-term post-transplant care. We strongly emphasize the importance of patients and caregivers educating themselves through these resources, as informed individuals are better equipped to work in partnership with the clinic to manage their condition effectively.
